DOJ Expands Healthcare Fraud Unit: Their #1 Target Are Providers and Those in Patient Care and the Life Sciences.
When you and your attorney commit to taking a case to trial, it’s because the strategy supports it. Trust in your counsel’s experience is crucial. And with a strong defense, acquittals are not just possible—they do happen.
- Not being a lawyer, my only advice is not to get on your judges’ bad side, as you may need them later for leniency. (i.e., No witness tampering).
-
Legal Representation Should Be Your First Decision: Fourteen Questions to Ask.
g
*
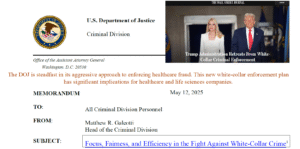
The DOJ’s New Enforcement: Data-Driven Era in Health Care Fraud
The Department of Justice’s Enforcement & Affirmative Litigation (EAL) initiative is reshaping how health care fraud is detected and prosecuted.
At its core, the Fraud Section’s Health Care Fraud Unit remains focused on two missions:
-
-
Protecting taxpayer-funded healthcare programs, such as Medicare, Medicaid, and TRICARE.
-
Protecting patients from fraudulent schemes that cause real harm, including the overprescribing of controlled substances.
-
A More Integrated, Data-Driven Approach
The DOJ’s new enforcement arm emphasizes an “integrated, data-driven, and swift” strategy that extends beyond traditional False Claims Act (FCA) cases. Enforcement now reaches into the life sciences industry, managed care organizations, private equity investments, and fintech-enabled health services — sectors where complex financial and data systems can obscure fraud risk.
Centralizing High-Impact Litigation
The EAL’s mission to “centralize high-impact affirmative litigation capabilities” means more efficient case selection and faster pursuit of credible leads. The goal: streamline investigations and maximize the impact of enforcement actions.
The Strike Force Model: Data Analytics at Work
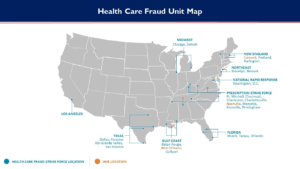
At the heart of this approach is the Strike Force Model, which utilizes advanced data analytics and algorithmic tools to uncover fraudulent activity. This includes:
-
-
Assessing scienter standards and causation frameworks in Anti-Kickback Statute cases.
-
Evaluating inducement evidence and remuneration valuation across marketing practices, consulting arrangements, and “value-add” incentives.
-
Examining medical necessity disputes and upcoding patterns through peer-comparison and physician-level outlier analysis.
-
Medicare Advantage Under Scrutiny
A central focus area is Medicare Advantage (MA). The DOJ is leveraging advanced analytics to review chart documentation, diagnosis coding, and risk adjustment data. These tools help identify inflated risk scores, unsupported hierarchical condition categories (HCCs), and retrospective coding initiatives that may distort program payments.
h
“ASCs Enter an Era of Accelerated Maturity by 2030”
The Next Phase for ASCs: Growth, Innovation, and Compliance
Ambulatory Surgery Centers (ASCs) are leading the shift toward high-quality, lower-cost surgical care — but as capabilities expand, so does federal scrutiny. With the DOJ’s data-driven Healthcare Fraud Enforcement Task Force intensifying oversight, ASC leaders must pair innovation with proactive compliance and transparency.
Bottom line:
Success in the next wave of outpatient care will depend not only on clinical excellence but on maintaining rigorous oversight of billing, referrals, quality reporting, and data integrity.
Key Trends Shaping the ASC Landscape:
-
-
Higher-acuity procedures: Orthopedic, spine, ENT, and GI cases continue shifting outpatient, increasing both opportunity and clinical risk.
-
Robotics & specialty equipment: More ASCs are investing or partnering to expand capabilities — requiring capital, training, and strong governance.
-
Payment & regulatory shifts: CMS updates and quality reporting rules are reshaping reimbursement models and compliance obligations.
-
Prior authorization expansion: New pilots and payer controls will heighten administrative and financial pressures.
-
Consolidation & strategic capital: Larger, joint-venture and PE-backed deals continue to drive scale, contracting leverage, and compliance complexity.
-
Workforce challenges: Staffing shortages, especially in anesthesia and perioperative roles, demand creative scheduling and cross-training models.
-
Technology integration: AI, advanced EHRs, and analytics are streamlining operations and enabling smarter patient selection — while also increasing the need for data governance.
-
Takeaway:
ASCs that align clinical growth with compliance, transparency, and data-driven oversight will be best positioned to thrive in an era of heightened regulatory focus.
><
o
THEIR FIRST TARGET IS YOU: WHITE-COLLAR HEALTHCARE, AND LIFE SCIENCES.
*
WHILE THE CHARGES TODAY ARE CIVIL AND FINANCIAL, TAKE THESE SERIOUSLY. CIVIL TODAY CAN BECOME CRIMINAL TOMORROW.
FIRST, GET LEGAL ADVICE.
A
SHOULD YOUR CHARGES BECOME CRIMINAL…
- WHETHER PLEA OR TRIAL
- CONSIDER ENGAGING MY SERVICES, YOUR 1st CONSULT IS ON ME. Dr. Blatstein, 240.888.7778
a
False Claims Act enforcement expands amid shifting white-collar landscape _ Reuters, 6/16/2025
A
CIVIL
From January 1 to May 31, 2025, the Department of Justice (DOJ) reported approximately 128 FCA settlements, totaling an impressive $1.257 billion, reflecting a robust enforcement strategy.
A
The Department of Justice (DOJ) has taken a bold step by filing a False Claims Act (FCA) lawsuit against major insurers—Aetna, Elevance, and Humana—alongside prominent brokers such as GoHealth, SelectQuote, and eHealth. This lawsuit exposes a deeply troubling scheme in which these insurance companies allegedly provided kickbacks to brokers, steering seniors towards Medicare plans that prioritize profits over genuine patient care. Such actions pose a grave threat to the integrity of our healthcare system and jeopardize the well-being of our most vulnerable seniors. The implications are profound, raising urgent questions about accountability and ethical standards in healthcare delivery.
A
Civil Rights Fraud Initiative
The memorandum directs the Department of Justice to vigorously pursue False Claims Act actions against any federal contractor or recipient of federal funds that knowingly infringes upon federal civil rights laws, particularly in matters concerning diversity, equity, and inclusion (DEI), including race, ethnicity, or national origin. In a bold move, President Trump has issued an Executive Order mandating federal and state agencies to implement measures that restrict access to medical treatments related to gender transition for minors, even with parental consent.
A
Scrutiny of Hospital–Physician Relationships Continues, 6/26/2025
A
⇑ DOJ MEMO TARGETS: HOSPITAL AND PHYSICIAN(CRIMINALLY) INDICTED ⇑
A
The federal government’s intense scrutiny of the relationships between hospitals and physicians is set to persist through 2025. It’s clear that healthcare fraud and abuse (as defined by DEI) remain among the highest priorities for federal oversight. This is a critical moment for healthcare providers to reassess and strengthen their compliance programs. By actively reviewing their policies and ensuring staff adherence, providers can take proactive steps to enhance compliance and protect their operations from potential legal repercussions.
A
Health Care Fraud Enforcement Under Trump 2.0
- Expect continued focus on healthcare fraud, the single largest driver of the federal government’s enforcement.
A
His Nominee
Dr. Mehmet Oz, the nominated Administrator for the Centers for Medicare and Medicaid Services (CMS), has described traditional Medicare as “highly dysfunctional.”
A
He has shown his support for Medicare Advantage while simultaneously expressing strong disapproval of traditional Medicare. In the realm of healthcare fraud enforcement, clinical laboratories are often scrutinized, particularly those involved in diagnostic and genetic testing, which may involve the performance of medically unnecessary tests. Additionally, Medicare payments for durable medical equipment (DME) and related medical supplies are frequently examined, with a focus on billing practices, coding accuracy, medical necessity, and potential kickbacks that could compromise the integrity of the system.
A
Health Care Fraud Law in the Courts
2024 underscored the importance of taking some instances to trial.
It is crucial to meticulously assess these issues at every stage: during the motion phase, throughout the trial, and, when necessary, on appeal. Fraud cases, especially those related to health care, frequently hinge on complex questions of intent that are best evaluated by a jury of one’s peers. This rigorous examination ensures justice is served and reinforces the integrity of the judicial process.
- United States v. Jeffrey Andrews, et. al., 2:20-cr-00578
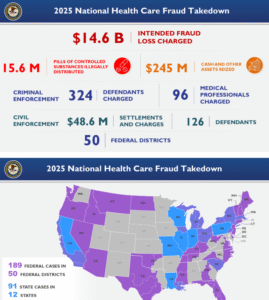
- National Health Care Fraud Takedown Results in 324 Defendants is just the beginning of the DOJ’s target on Healthcare.
- Medicare Advantage (patients believe that it is “exactly” the same as Medicare, which isn’t so).
- United Healthcare is facing a plethora of litigation.
A
MY TAKEAWAY – MY RECOMMENDATION
A
Risk-Adjustment Coding in 2025:
S
S
A
A
In 2025, commercial insurers, particularly those managing Patient Protection and Affordable Care Act (PPACA) marketplace plans and employer-based products, are heavily relying on risk-adjusted payment models.
- This evolution is here,
-
- Health Information Management (HIM) professionals and
- Coding Teams into new territory, where
- Documentation Integrity,
- Chronic Disease Capture, and
- Accurate Coding is essential
- Clinical Documentation Improvement (CDI)
- Expand CDI efforts beyond inpatient settings to focus on physician offices, clinics, and telehealth visits;
- Pre-visit planning
- Chart auditing: Regular
- Advanced Data Analytics and Artificial Intelligence (AI)-driven coding support tools can greatly assist, but do not replace clinical judgment and coding expertise.
- The integrity of the data remains a human responsibility.
C
This is a statistical process that modifies payments based on a patient’s disease burden and demographic risk.
Conclusion,
- Risk adjustment has matured from a niche Medicare concern into a universal driver of revenue, quality, and compliance across the healthcare continuum.
- More or as Important: this appears to be a legal defense necessity.
- Don’t underestimate the value of your hard work and attention to detail. You’ll see the true impact of your efforts after your counsel reviews your charges and documentation. Their confidence after reviewing your records will highlight the significance of what you’ve accomplished.
- This preparation will be invaluable as you head into your meeting with the DOJ, reinforcing just how crucial your dedication has been in this process.
A
WHILE THE CHARGES MAY START CIVIL (FINANCIAL), TAKE THESE SERIOUSLY.
CIVIL TODAY CAN BECOME CRIMINAL TOMORROW.
FIRST, GET LEGAL ADVICE.
A
SHOULD CHARGES BECOME CRIMINAL
- WHETHER PLEA OR TRIAL
- CONSIDER ENGAGING MY SERVICES, YOUR 1st CALL IS ON ME.
- Dr. Blatstein
Physician Presentence Report Service
240.888.7778
PPRSUS.com
PHYSICIAN PRISON CONSULTANT
WHITE-COLLAR, SENTENCE MITIGATION SOLUTIONS
S