THE DOJ 1st TARGET FRAUD: HEALTHCARE PROVIDERS – TELEHEALTH – PHARMA – DIGITAL AI
*
WHITE-COLLAR PROVIDER SPECIALISTS – TELEHEALTH – PHARMA.
*
WHILE THE CHARGES MAY START CIVIL (FINANCIAL), TAKE THESE SERIOUSLY. CIVIL TODAY CAN BECOME CRIMINAL TOMORROW.
FIRST, GET LEGAL ADVICE.
A
A
SHOULD YOUR CHARGES BECOME CRIMINAL
-
- WHETHER BY PLEA OR TRIAL,
- CONSIDER ENGAGING MY SERVICES, YOUR 1st CALL IS ON ME. Dr. Blatstein, 240.888.7778
May 12, 2025
MEMORANDUM
TO: All Criminal Division Personnel
FROM: Matthew R. Galeotti
Head of the Criminal Division
SUBJECT: Focus, Fairness, and Efficiency in the Fight Against White-Collar Crime
#1: HEALTHCARE
S
A
I. DOJ EXPANDS TELEHEALTH ENFORCEMENT | Advisories
A
A
*
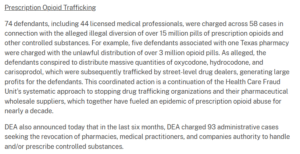
DOJ’s Current Telehealth Enforcement Actions Target Prescription Opioid Trafficking
z
A
A
Medical practitioners are increasingly prescribing items and services to patients who have been identified and recruited through telemedicine companies.
Medical practitioners who are compensated based on the volume of prescriptions they write, or through other methods that may incentivize the unnecessary ordering of items or services, can compromise the integrity of patient care and lead to detrimental outcomes.
Subpar patient engagement, characterized by minimal interaction and a lack of thorough examination, coupled with a troubling absence of follow-up expectations for patients.
Inconsistent medical practices, marked by a narrow range of product offerings and significant restrictions on treatment options, undermine the quality of care provided.
A
Internal Company Controls
- It is imperative to thoroughly verify prescription medications prior to dispensing to ensure patient safety.
- Compensation arrangements must never compromise the integrity of independent physician-patient relationships.
- Key warning signs include the absence of a previous in-person relationship with the provider.
- Patients should have the clear right to cancel services without any obstacles.
A
II. SPECIALTIES – WOUND CARE
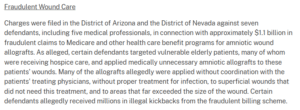
Fraudulent Wound Care
Charges were filed against seven defendants, including five medical professionals, in connection with approximately $1.1 billion in fraudulent claims submitted to Medicare and other healthcare benefit programs for amniotic wound allografts.
R
A
Numerous allografts were reportedly used without proper coordination with the patients’ physicians, often applied without adequate infection treatment, and to superficial wounds that didn’t need it. This reflects a concerning disregard for medical protocols and patient care standards.
It’s never too late to begin paying attention to the detailed patient documentation of your team or colleagues.
a
A
⇑ RISK ADJUSTMENT CODING INCLUDES DOCUMENTATION- CLEAR CHARTING- INTERNAL AUDITS ⇑
S
Wound Care in the Crosshairs: Risks Amid Skin Substitute Fraud Investigations
- Effective wound care is essential for patients recovering from surgery or managing chronic and non-healing wounds.
- Advances in treatment have led to the development of skin substitutes—bioengineered or natural materials designed to promote healing by replacing or supporting damaged skin.
- However, concerns regarding clinical efficacy, medical necessity, and appropriate use have intensified scrutiny of the agreements between healthcare providers and skin substitute distributors and manufacturers, particularly in light of potential fraud.
- Unfortunately, many healthcare providers who offer legitimate and necessary treatments for their patients have found themselves caught in the midst of this scrutiny.
- Medicare has increased its review of wound care billing, identifying it as high-risk for fraud, overpayment, and misuse.
- As a result, there has been a significant rise in government audits and investigations targeting wound care services and the use of skin substitutes.
A
III. TELEMEDICINE, DME, GENETIC TESTING FRAUD, and DIGITAL HEALTH
As digital health delivery models continue to gain traction, it is likely that remote prescribing arrangements will not be the only targets for fraud in this evolving landscape. Additionally, in the realm of behavioral health, a rule finalized by the Centers for Medicare & Medicaid Services (CMS) last year has established that, beginning January 1, 2025, Medicare will provide coverage for specific mental health apps. This development represents a significant step toward expanding access to mental health services through digital platforms.
A

⇑ RISK ADJUSTMENT CODING INCLUDES DIGITAL SECURITY ⇑
Z
DME
Prosecutors in the Southern District of Florida have charged the owner of telemedicine and medical equipment companies for submitting fraudulent Medicare claims related to durable medical equipment and genetic tests, exploiting vulnerable beneficiaries.
A
Pharma
The DOJ “remains committed to thoroughly pursuing allegations of price fixing and kickbacks that put the Medicare program at risk.” Notably, FCA actions target the Pharmaceutical Manufacturer Patient Assistance Programs.
Pharmacy Benefit Managers
Often referred to as “intermediaries” in the pharmaceutical industry, PBMs negotiate drug prices with pharmacies and manufacturers, establish drug tiers, and determine reimbursement rates.
A
IV. YOUR PRACTICE – RISK ADJUSTMENTS INCLUDE DOCUMENTATION
Providers can take several proactive steps to mitigate audit risk and enhance reimbursement outcomes when utilizing skin substitutes. Here are some recommendations:
- **Thorough Documentation**: It is essential that the documentation is comprehensive and clearly supports the medical necessity for using skin substitutes, especially when advanced products such as cellular or tissue-based grafts are involved. Given that these products may have limited clinical research backing their use, detailed notes on the patient’s condition, treatment history, and the rationale for selecting these advanced options are crucial. This should include specific clinical indicators that justify their use.
- **Patient Chart Clarity**: Each patient’s medical chart should include explicit reasoning for why the standard of care was insufficient. Providers should articulate the unique aspects of the patient’s case that necessitated continued treatment with skin substitutes. It’s important to be aware of the proposed Local Coverage Determinations (LCDs) set to take effect on January 1, 2026, which will permit only 8 applications of skin substitutes within a maximum treatment period of 16 weeks. Although these rules are not yet in effect, providers should begin to prepare and document any justifications for extending treatment beyond these parameters where clinically justified.
- **Regular Internal Audits**: Conducting routine internal audits focusing on high-risk billing codes is advisable. Providers should develop an understanding of the current LCD guidelines and ensure they remain informed about Medicare’s continually evolving regulations and guidelines. This proactive measure will not only help in identifying potential compliance issues before they arise but also aid in training staff on appropriate billing practices.
- **Review Agreements with Manufacturers**: Providers should conduct thorough reviews of their agreements with manufacturers and distributors of skin substitutes. This evaluation is crucial for identifying and mitigating potential exposure to violations of federal or state Anti-Kickback Statutes. It’s crucial to ensure that any relationships with suppliers are transparent and compliant with all regulatory requirements to avoid legal repercussions.
By implementing these strategies, providers can not only reduce their audit risks but also improve their chances of obtaining appropriate reimbursement for skin substitute treatments.
A
MY TAKEAWAY RECOMMENDATION, DECREASE RISK
A
Risk-Adjustment Coding in 2025:
A
A
A
⇑ TO READ THE FULL ARTICLE HERE: CLICK LINK IN PIC., ABOVE ⇑
A
In 2025, commercial insurers, particularly those managing Patient Protection and Affordable Care Act (PPACA) marketplace plans and employer-based products, are heavily relying on Risk-Adjusted Payment Models.
- This evolution is here,
-
- Health Information Management (HIM) professionals and
- Coding Teams into new territory, where
- Documentation Integrity,
- Chronic Disease Capture, and
- Accurate Coding is essential
- Clinical Documentation Improvement (CDI)
- Expand CDI efforts beyond inpatient settings to focus on physician offices, clinics, and telehealth visits;
- Pre-visit planning
- Chart auditing: Regular
- Advanced Data Analytics and Artificial Intelligence (AI)-driven coding support tools can greatly assist, but do not replace clinical judgment and coding expertise.
- The integrity of the data remains a human responsibility.
This is a statistical process that modifies payments based on a patient’s disease burden and demographic risk.
Conclusion,
- Risk adjustment has matured from a niche Medicare concern into a Universal Driver of Revenue, Quality, and Compliance across the Healthcare Continuum.
- More or as Important: this appears to be a legal defense necessity.
- Right now, the value of your hard work and attention to detail is becoming clear.
- After your counsel’s thorough examination of your records, you’ll truly understand the impact of your attention to documentation detail. As they recognize your efforts, the weight you’ve been carrying will lift, restoring your confidence.
- This preparation will be invaluable as you head into your next meeting with the DOJ, reinforcing just how crucial your dedication has been in this process.
WHILE THE CHARGES MAY START CIVIL (FINANCIAL), TAKE THESE SERIOUSLY. CIVIL TODAY CAN BECOME CRIMINAL TOMORROW.
FIRST, GET LEGAL ADVICE.
A
THEN IF CRIMINAL,
-
- WHETHER PLEA OR TRIAL
- CONSIDER ENGAGING MY SERVICES.
- YOUR 1st CALL IS ON ME.
- Dr. Blatstein
Physician Presentence Report Service
240.888.7778
PPRSUS.com
PHYSICIAN PRISON CONSULTANT
WHITE-COLLAR, SENTENCE MITIGATION SOLUTIONS
S