PROTECT YOUR LIFE: PRISON MEDICAL CARE DELAYED, COULD BE TOO LATE.
WHY TOO LATE?
FEDERAL Judge Roy Dalton Holds Federal Bureau of Prisons in Contempt.
-
FCI Seagoville, a low-security federal correctional facility where Bardell is housed, has been the hardest hit federal prison in the nation by the COVID-19
-
October 10, 2022, Judge Holds Federal Bureau of Prisons in Contempt for Allowing Man To Waste Away From Untreated Cancer.

SEEING A SPECIALIST IS A WISH AND USUALLY NEVER TIMELY
a
THE AMERICAN ACADEMY OF ORTHOPEDICS
Traumatic Orthopaedic Injuries in the Prison Population
w
Barreto Rocha, Daniela MD; Sanchez, Daniela MD; Grandizio, L. Christopher DO; Maniar, Hemil Hasmukh MD; Horwitz, Daniel Scott MD
w
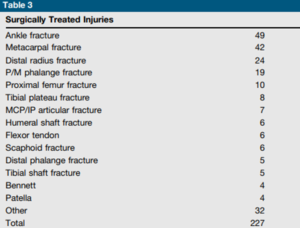
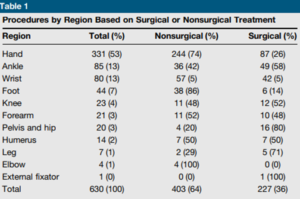
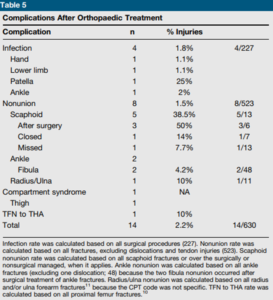
RESULT:
- The hand and wrist were the most commonly injured regions (65%), followed by the foot and ankle (20%). Metacarpal fractures represented 22% of all injuries. A low complication rate was noted among all surgical procedures. Infection was seen in 1.15% of hand surgeries and 2% of ankle surgeries. In addition, a low incidence of nonunion was recorded (1.5%).
w
- Nonsurgical management was the chosen treatment method in 64% of all injuries.
NATIONAL LIBRARY of MEDICINE
I. Injuries Associated with Bunk Beds that Occur in Jail
Forensic Leg Med., 2018 Randall T Loder, Jocelyn Cole Young
 Conclusions:
Conclusions: - Injuries in jail account for 29% of all bunk bed injuries resulting in an ED visit in the USA in those age groups ≥10 years. A fall from the bed occurred in 72%, and a seizure disorder was 4.5 times more common in jail inmates.
- You had a recent joint replacement or other surgery or a medical condition that addresses instability, cognition decline, instability, or tinnitus, and your physician records in your Presentence Report should note that you Should only be placed in a Lower Bunk – not an Upper Bunk. If a fall results from that upper bunk in a fractured hip followed by, at best, delayed care, this could be an end-of-life event.
a
II. Mortality and cause of death in hip fracture patients aged 65 or older – a population-based study
- The average follow-up period was 3.7 years, from 0 to 9 years. The one-year postoperative mortality rate was 27.3%, and by the end of the follow-up period, the mortality rate following a hip fracture had risen to 79.0%. Age-adjusted mortality after hip fracture surgery was found to be higher in men, with a hazard ratio of 1.55 (95% CI 1.21-2.00).
- The primary causes of death among patients who underwent hip surgery were circulatory diseases, followed by dementia and Alzheimer’s disease. Additionally, men were more likely than women to die from respiratory diseases and malignant neoplasms following a hip fracture. Overall, the age- and sex-adjusted mortality rate after hip fracture was three times higher than that of the general population.
a
IF YOU ARE NOT SURE WHAT TO DO FIRST, START WITH A FREE CONSULTATION FOR YOU OR A LOVED ONE. THIS IS MY CELL, 240.888.7778, AND I ANSWER AND RETURN ALL MY CALLS.
OTHER COMMON FOOT AND ANKLE INJURIES
I. PLANTAR FASCIITIS
a
- Chief complaint: Patients experience pain upon standing first thing in the morning. While the pain initially is excruciating, with ambulating, the pain may subside, only to come back again with a vengeance after sitting and then immediately return after standing up again.
- Even when a bone spur is present, that is usually not the cause of the pain unless other pathology is evident.
- The plantar fascia is a ligament attached at one end to the bottom of the heel (in a medial, central, and lateral band), then fanning out into the ball of the foot, thus acting as a shock absorber for the foot. As the foot impacts the ground, the plantar fascia stretches slightly with each step. When these excessive pressures of pulling the plantar fascia on the heel occur over time, with an innocent step (like stepping on a marble or off a curb), they create small tears in the plantar fascia (the ligament on the bottom of the foot) resulting in a small amount of bleeding, pain & inflammation.
a
II. PAINFUL HAMMERTOE

- Hammertoes appear with the toes bent in a clawing fashion. They may be flexible or rigid; flexible infers that you can manually straighten the toes, while it is impossible to straighten the rigid toe without surgery. Because most of us wear enclosed shoe gear, the pressure caused by the shoe gear causes the toes to become painful.
- Dr. Marc Blatstein recommends a combination of appropriate shoe gear and a functional orthotic prescribed as a shoe insert to help the hammertoes from progressing or worsening. In the very initial stages, while the toe is still flexible, it can
 be tapped into its corrected position, utilizing a functional orthotic. This conservative treatment also consists of hammertoe and buttress pads, all available over the counter, and open-toe shoes.
be tapped into its corrected position, utilizing a functional orthotic. This conservative treatment also consists of hammertoe and buttress pads, all available over the counter, and open-toe shoes.
While successful in correcting a deformity with continued pain, it depends on whether it is rigid or flexible. With a rigid hammertoe, the surgical procedure consists of removing some skin and a small section of bone. Following your surgeon’s after-surgery instructions is essential to getting the best result.
a
III. TARSAL TUNNEL (ANKLE) OR CARPAL TUNNEL(THE WRIST) SYNDROME
- Tarsal Tunnel Syndrome is due to the compression of a nerve called
 the Posterior Tibial Nerve. Tarsal Tunnel Syndrome occurs over time as the nerve becomes inflamed, resulting in symptoms such as burning, electric shocks, and tingling, as well as a shooting type of pain. Other factors that Dr. Marc Blatstein has found factors contributing to Tarsal Tunnel Syndrome come from either an overly pronated foot, which puts a stretch on the nerve, pressure on the nerve from soft tissue masses such as ganglions, fibromas, or lipomas that physically compress the nerve, as well as other insults to the nerve.
the Posterior Tibial Nerve. Tarsal Tunnel Syndrome occurs over time as the nerve becomes inflamed, resulting in symptoms such as burning, electric shocks, and tingling, as well as a shooting type of pain. Other factors that Dr. Marc Blatstein has found factors contributing to Tarsal Tunnel Syndrome come from either an overly pronated foot, which puts a stretch on the nerve, pressure on the nerve from soft tissue masses such as ganglions, fibromas, or lipomas that physically compress the nerve, as well as other insults to the nerve.
a
Treatment of the Tarsal Tunnel involves many different components, some of which are correcting the  abnormal pronation of the foot [which is accomplished with prescription functional foot orthotics]. Along with this, oral anti-inflammatory medications, vitamin B supplements, &/or steroids may provide some benefit but are rarely curative. Should a soft tissue mass compress the nerve, surgical removal of the mass may be necessary. Surgical correction of Tarsal Tunnel Syndrome has a good chance of success; at the same time, the overpronation of the foot still needs to be followed with functional foot orthotics.
abnormal pronation of the foot [which is accomplished with prescription functional foot orthotics]. Along with this, oral anti-inflammatory medications, vitamin B supplements, &/or steroids may provide some benefit but are rarely curative. Should a soft tissue mass compress the nerve, surgical removal of the mass may be necessary. Surgical correction of Tarsal Tunnel Syndrome has a good chance of success; at the same time, the overpronation of the foot still needs to be followed with functional foot orthotics.
a
IV. STRESS OR HAIRLINE FRACTURES
- It can only be seen on X-ray after 2 weeks when the hairline fracture is healing.
- A stress fracture may be seen earlier; next is to ensure the bones are aligned.
 The name “March” Fracture is used as these usually occur after long marches and are caused by repetitive force, often from overuse—such as repeatedly jumping up and down or running long distances over time.
The name “March” Fracture is used as these usually occur after long marches and are caused by repetitive force, often from overuse—such as repeatedly jumping up and down or running long distances over time.
- If it’s in a Metatarsal, usually the 2nd is the longest, but the 5th could
 also be the bone involved. A surgical shoe has a rigid, flat bottom and helps most foot injuries heal quicker. The Darco shoe is one example.
also be the bone involved. A surgical shoe has a rigid, flat bottom and helps most foot injuries heal quicker. The Darco shoe is one example.
a
V. ANKLE SPRAINS, v. TRI-MALLEOLAR ANKLE FRACTURE, FEATURED IMAGE ABOVE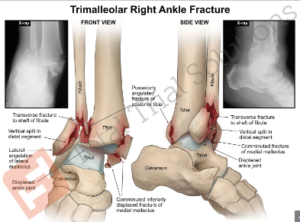
ANKLE SPRAIN: LIGAMENTS. Ligaments attach bone to bone; the ankle sprain and ligaments inside the ankle are very strong and could fracture the bone.
a

a
RICE
-
- Rest: Avoid walking on the ankle.
- Ice: To reduce swelling, apply ice for 20–30 minutes, 3–4 times daily.
- Compression: To support and immobilize the ankle, use a compression bandage like a 3″, 4″, or 6″ ACE Wrap.
- Elevation: Keep the ankle above the heart for at least 48 hours.
- Pain relievers: Take over-the-counter pain relievers like ibuprofen, naproxen sodium, or acetaminophen
- With no improvement, you should seek medical care.
a
VI. ACHILLES TENDON INJURIES
- The tendon attaches the muscle to the bone; the Achilles could wholly or partially tear with the muscle. For both, the remaining tendon muscle complex retracts proximally. This is a severe and painful injury that will also affect your ability to stand – medical care is a must.

a
The common theme is that federal prisons, and prisons in general, only provide the most basic care, so do not count on getting medical care like you are used to at home. It is okay to play sports; just do not get seriously hurt, as seeing a specialist may take years, if at all.
a
VII. ACTION STEPS TO TAKE TO KEEP YOUR LIFE AND HEALTH
- YOUR MEDICAL FILE ONLY ‘INDICATES’ THAT YOUR MEDICAL AND SURGICAL HISTORY INDICATES A LOWER BUNK. CHANGE THAT! IT NEEDS TO READ, NO UPPER BUNK.
- YOU WANT TO PLAY SPORTS, GREAT. IF YOU’RE A ‘SHORT-TIMER’ AND HAVE A PENDING CONTRACT OF GREATER THAT $1M IN THE LEAGUE OF YOUR CHOICE, OR EVEN IF YOU DON’T, UNDERSTAND THAT HEALTHCARE IN PRISON IS NOT LIKE IT IS AT HOME.
- FOR EXAMPLE, SECOND-OPINION SPECIALISTS CAN TAKE YEARS TO WAIT, AND THEN THE BOP IS NOT OBLIGATED TO FOLLOW THEIR RECOMMENDATIONS. READ MY ARTICLE: Availability of Treatment and Rehabilitation in Federal Prison: The Critical Role of the Presentence Report
- IN PRISON, USE THE ADMINISTRATIVE REMEDY PROCESS: BP 8-11, §2241, §2255
- PART I) FOR ALL GRIEVANCES AND ACTION STEPS THE INMATE CAN TAKE.
- PART II) COVERS STEPS THE FAMILY (OR THOSE WITH POA) CAN TAKE.
VIII. SCOPE OF SERVICES – CATEGORIES OF CARE (Pages 5-8)
Medically Necessary – Acute or Emergent.
- Myocardial infarction.
- Severe trauma, such as head injuries.
- Hemorrhage.
- Stroke.
- Status asthmaticus.
- Precipitous labor or complications associated with pregnancy.
- Detached retina, sudden loss of vision.
Medically Necessary – Non-Emergent.
- Serious deterioration leads to premature death.
- Significant reduction in the possibility of repair later without present treatment.
- Significant pain or discomfort which impairs the inmate’s participation in activities of daily living
- Chronic conditions (diabetes, heart disease, bipolar disorder, schizophrenia).
- Infectious disorders in which treatment allows for a return to a previous state of health or improved quality of life (HIV, tuberculosis).
- Cancer.
Medically Acceptable – Not Always Necessary.
- Joint replacement.
- Reconstruction of the anterior cruciate ligament of the knee.
- Treatment of non-cancerous skin conditions (e.g., skin tags, lipomas).
- The risks and benefits of the treatment.
- Available resources.
- Natural history of the condition.
- The effect of the intervention on inmate functioning in his/her activities of daily living.
Limited Medical Value.
- Minor conditions that are self-limiting.
- Cosmetic procedures (e.g., blepharoplasty).
- Removal of non-cancerous skin lesions.
Extraordinary.
- They affect the life of another, such as organ transplantation
Then, each request goes through each individual facility’s established Utilization Review Committee’s (URC) Policy.